IN THIS LESSON
This review aims to critically evaluate the current evidence regarding photobiomodulation's efficacy and mechanisms of action in treating neurodegenerative diseases, with particular emphasis on addressing key questions about light penetration and optimal treatment parameters. Specifically, the review seeks to:
Examine the physical principles and limitations of near-infrared light penetration through biological tissues, particularly focusing on the crucial differences between low-power LED devices versus high-powered laser systems in achieving therapeutic fluence levels in deep brain structures.
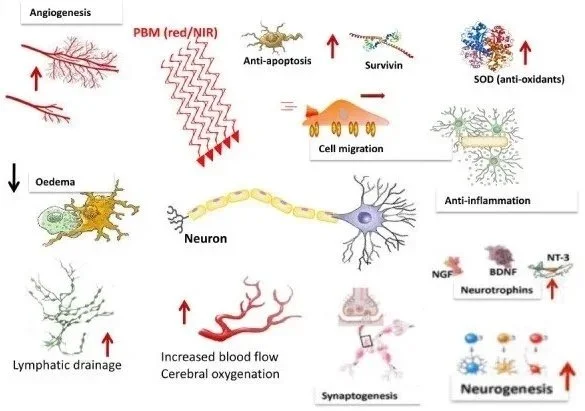
Analyze the reported mechanisms through which photobiomodulation influences neuronal function and survival, including both direct effects on cellular metabolism and indirect systemic effects through circulatory systems.
Evaluate existing preclinical and clinical evidence for the therapeutic efficacy of photobiomodulation in neurodegenerative conditions, particularly Alzheimer's disease and Parkinson's disease.
This review addresses critical gaps in current understanding:
Clarifying misconceptions about light penetration capabilities of different devices
Providing evidence-based analysis of required power densities and fluence levels needed to achieve therapeutic effects in deep brain tissue
Examining whether reported clinical benefits align with our understanding of light penetration physics.
-
Citations:
Henderson TA, Morries LD. Near-infrared photonic energy penetration: can infrared phototherapy effectively reach the human brain? Neuropsychiatr Dis Treat. 2015;11:2191-2208.
Morries LD, Cassano P, Henderson TA. Treatments for traumatic brain injury with emphasis on transcranial near-infrared laser phototherapy. Neuropsychiatr Dis Treat. 2015;11:2159-75.
Henderson TA, Morries LD. Multi-watt near-infrared phototherapy for the treatment of comorbid depression: An open-label single-arm study. Front Psychiatry. 2017;8:187.
Shen Q, Guo H, Yan Y. Photobiomodulation for neurodegenerative diseases: A scoping review. Int J Mol Sci. 2024;25:1625.
Moro C, Valverde A, Dole M, et al. The effect of photobiomodulation on the brain during wakefulness and sleep. Front Neurosci. 2022;16:942536.
Hamblin MR. Shining light on the head: Photobiomodulation for brain disorders. BBA Clin. 2016;6:113-124.
Lapchak PA, Boitano PD, Butte PV, et al. Transcranial near-infrared laser transmission (NILT) profiles: Systematic comparison in four common research species. PLoS ONE. 2015;10:e0127580.
Cassano P, Petrie SR, Hamblin MR, et al. Review of transcranial photobiomodulation for major depressive disorder: targeting brain metabolism, inflammation, oxidative stress, and neurogenesis. Neurophotonics. 2016;3:031404.
Tedford CE, DeLapp S, Jacques S, Anders J. Quantitative analysis of transcranial and intraparenchymal light penetration in human cadaver brain tissue. Lasers Surg Med. 2015;47:312-22.
Barrett DW, Gonzalez-Lima F. Transcranial infrared laser stimulation produces beneficial cognitive and emotional effects in humans. Neuroscience. 2013;230:13-23.
Salehpour F, Rasta SH, Mohaddes G, et al. Therapeutic effects of 10-Hz pulsed wave lasers in rat depression model: A comparison between near-infrared and red wavelengths. Lasers Surg Med. 2016;48:695-705.
Naeser MA, Zafonte R, Krengel MH, et al. Significant improvements in cognitive performance post-transcranial, red/near-infrared light-emitting diode treatments in chronic, mild traumatic brain injury: open-protocol study. J Neurotrauma. 2014;31:1008-17.
Xuan W, Agrawal T, Huang L, et al. Low-level laser therapy for traumatic brain injury in mice increases brain-derived neurotrophic factor (BDNF) and synaptogenesis. J Biophotonics. 2015;8:502-11.
Johnstone DM, Moro C, Stone J, et al. Turning on lights to stop neurodegeneration: The potential of near-infrared light therapy in Alzheimer's and Parkinson's disease. Front Neurosci. 2016;9:500.
Wang X, Tian F, Reddy DD, et al. Up-regulation of cerebral cytochrome-c-oxidase and hemodynamics by transcranial infrared laser stimulation: A broadband near-infrared spectroscopy study. J Cereb Blood Flow Metab. 2017;37:3789-3802.